Autoimmune conditions are on the rise, affecting millions of people globally. For many, the path to healing can feel like a confusing maze of symptoms, specialists, and prescriptions. But what if we stopped chasing symptoms and started uncovering root causes? What if healing was about bringing the whole body back into balance, physically, mentally, and emotionally?
That’s the heart of my upcoming course, A Holistic Approach to Autoimmune Disorders. In this blog post, I’ll be walking you through 9 often-overlooked root causes that can contribute to autoimmune dysfunction. Understanding these factors is the first step in reclaiming your health. Whether you're newly diagnosed or years into your journey, this knowledge can help you make powerful, informed changes that support your body’s natural ability to heal.
Let’s start with the first root cause: leaky gut.
1. Leaky Gut: The Gateway to Chronic Inflammation
Your gut isn't just where food is digested. It's also where your immune system lives. In fact, around 70% of your immune cells are housed in the gut lining. When that lining becomes damaged, a condition known as “leaky gut” or intestinal permeability, it can let undigested food particles, toxins, and microbes leak into the bloodstream. The immune system sees these intruders and launches an attack.
Over time, this constant immune activation can confuse the body, leading it to mistakenly attack its own tissues. This is one of the core mechanisms behind autoimmune disease.
Common causes of leaky gut:
-
Overuse of antibiotics or NSAIDs (like ibuprofen)
-
Processed foods and refined sugars
-
Chronic stress
-
Imbalanced gut bacteria
-
Gluten and other inflammatory foods
Signs you may have a leaky gut:
-
Bloating, gas, or IBS symptoms
-
Skin issues like eczema or acne
-
Food sensitivities
-
Brain fog or fatigue
-
Joint pain
Healing the gut is often the first and most important step in addressing autoimmune disease holistically. This means removing irritants, repairing the gut lining with targeted nutrients, and restoring balance to the microbiome. Learn more in my 20 Module course, Holistic Approaches to Gut Health.
 2. Food Sensitivities: When “Healthy” Foods Hurt
2. Food Sensitivities: When “Healthy” Foods Hurt
Food is supposed to nourish us. But for someone with an autoimmune condition, even foods that are technically healthy can trigger inflammation and make symptoms worse. This is because of something called food sensitivities—a delayed, immune-mediated reaction to certain foods that your body starts to perceive as threats.
Unlike a food allergy, which can cause immediate and severe reactions, food sensitivities often show up hours or even days after eating. That delay makes them tricky to spot, but they can silently contribute to ongoing immune system activation and inflammation.
What causes food sensitivities?
Food sensitivities are often the result of leaky gut. When the gut lining is compromised, food particles can enter the bloodstream before they’re fully broken down. The immune system, always on guard, sees these particles as invaders and creates antibodies against them. Over time, this can lead to a long list of sensitivities—even to foods you’ve eaten your whole life without issue.
Common culprits include:
-
Gluten
-
Dairy (especially casein)
-
Soy
-
Eggs
-
Corn
-
Nightshades (like tomatoes, peppers, and eggplant)
-
Nuts and seeds (for some people)
Signs you might have food sensitivities:
-
Digestive issues (bloating, gas, constipation, diarrhea)
-
Headaches or migraines
-
Skin problems (rashes, hives, eczema)
-
Joint or muscle pain
-
Fatigue and brain fog
-
Anxiety or mood swings
How to identify them:
While food sensitivity tests can offer some clues, they're not always reliable. One of the most effective ways to uncover your personal triggers is through an elimination diet—a short-term, strategic plan where you remove common offenders and then reintroduce them one at a time to observe how your body reacts.
This isn’t about restriction for the sake of restriction. It’s about giving your body a break from foods that may be keeping it in a state of constant inflammation. Once the gut is healed and the immune system calms down, many people find they can tolerate more foods again.
Quick Recap: Food Sensitivities
-
Often caused by leaky gut and immune overactivation
-
Symptoms can appear hours or days later, making them hard to pinpoint
-
Elimination diets are a powerful tool for identifying triggers
 3. Chronic Infections: The Hidden Burden on Your Immune System
3. Chronic Infections: The Hidden Burden on Your Immune System
We tend to think of infections as something short-term, like a cold or flu. But many people with autoimmune conditions are dealing with low-grade, chronic infections that linger under the surface. These infections may not cause obvious symptoms, but they keep the immune system on constant alert, like a smoke alarm that never stops.
Over time, this ongoing immune activation can confuse the body and cause it to target its own tissues—a core issue in autoimmunity.
Common chronic infections linked to autoimmunity:
-
Epstein-Barr Virus (EBV)
-
Herpes Simplex Virus (HSV)
-
Cytomegalovirus (CMV)
-
Candida overgrowth
-
Small Intestinal Bacterial Overgrowth (SIBO)
-
Tick-borne illnesses (Lyme, Babesia, Bartonella)
How they contribute to autoimmune conditions:
Chronic infections create inflammation and sometimes molecular mimicry, where the body confuses its own tissues with the pathogen. For example, EBV has been linked to Hashimoto’s and MS, candida overgrowth can worsen psoriasis, and SIBO is common in rheumatoid arthritis and celiac disease.
Signs of a chronic infection:
-
Fatigue that doesn’t improve with rest
-
Brain fog or poor memory
-
Muscle or joint pain
-
Frequent sore throats or swollen glands
-
Skin flare-ups or rashes
-
Symptoms that worsen after stress or illness
What helps:
Support your immune system with rest, nutrition, and stress reduction. Then, work with a practitioner to gently address chronic infections using immune support, gut healing, and herbal therapies if needed.
Quick Recap: Chronic Infections
-
Low-level infections can keep the immune system in overdrive
-
Linked to many autoimmune conditions through inflammation and mimicry
-
Gentle detox and immune support are key
 4. Nutrient Deficiencies: When the Body Doesn’t Have the Tools to Heal
4. Nutrient Deficiencies: When the Body Doesn’t Have the Tools to Heal
Imagine trying to build a house without wood, nails, or a solid foundation. That’s what healing is like without key nutrients. Even with a healthy diet, nutrient deficiencies are common in autoimmune conditions and can seriously slow your progress.
Why deficiencies are so common:
-
Leaky gut and poor nutrient absorption
-
Chronic inflammation depleting key vitamins and minerals
-
Medications like antacids, NSAIDs, steroids, and birth control
-
Soil depletion and modern farming practices
-
Restrictive diets that eliminate entire food groups
Key nutrients for immune and gut health:
-
Vitamin D
-
Zinc
-
Magnesium
-
Omega-3 fatty acids
-
B vitamins and iron
-
Selenium and iodine
Signs of deficiency:
-
Fatigue or low energy
-
Brain fog or mood swings
-
Poor wound healing
-
Hair loss or brittle nails
-
Muscle cramps
-
Feeling cold or signs of low thyroid function
What to do:
Start with a nutrient-rich, whole foods diet. Consider testing to find specific deficiencies and supplement as needed, ideally with the guidance of a practitioner. Replenishing nutrients helps restore immune balance and supports energy, mood, and healing.
Quick Recap: Nutrient Deficiencies
-
Common due to inflammation, gut issues, and medications
-
Can impact every system related to autoimmunity
-
Testing and targeted support can make a big difference
 5. Insulin Surges: The Blood Sugar and Inflammation Connection
5. Insulin Surges: The Blood Sugar and Inflammation Connection
We don’t often link blood sugar to autoimmune disease, but keeping blood sugar stable is essential for immune balance. Frequent insulin surges—caused by sugar spikes—can drive inflammation and disrupt hormone and immune function.
Here’s what happens:
You eat something high in sugar or refined carbs. Blood sugar rises quickly. Insulin rushes in to bring it down. Repeat this cycle often enough, and you can become insulin resistant.
How insulin surges impact autoimmunity:
-
Increase inflammation, especially in joints and the brain
-
Trigger cortisol release, which over time worsens immune dysregulation
-
Disrupt hormone balance
-
Lead to fatigue, mood swings, and brain fog
-
Increase the chance of autoimmune flares
What causes blood sugar spikes:
-
High-carb, low-protein meals
-
Sugary snacks and drinks
-
Skipping meals
-
Coffee on an empty stomach
-
Chronic stress
Signs your blood sugar is out of balance:
-
Cravings for sugar or carbs
-
Energy crashes after meals
-
Feeling shaky or irritable between meals
-
Difficulty sleeping
-
Belly fat
How to support blood sugar balance:
-
Start your day with protein and healthy fat
-
Eat regularly and don’t skip meals
-
Balance each meal with protein, fiber, and fat
-
Limit refined sugar and processed carbs
-
Move after meals to support insulin function
Quick Recap: Insulin Surges
-
Blood sugar instability drives inflammation and hormone imbalance
-
Even without diabetes, it can affect autoimmune flares
-
Balance comes from real food, regular meals, and stress management
 6. Toxins and Chemicals: The Invisible Burden on the Immune System
6. Toxins and Chemicals: The Invisible Burden on the Immune System
We’re exposed to environmental toxins every day. From pesticides in food to plastics, fragrances, and mold, these chemicals can overload our body’s detox systems and push the immune system into overdrive.
Common toxin sources:
-
Pesticides (especially in non-organic produce)
-
Heavy metals like mercury
-
Mold toxins from water-damaged buildings
-
BPA and phthalates from plastics
-
Synthetic fragrances in personal care and cleaning products
-
Hormone-disrupting chemicals in skincare
How toxins contribute to autoimmunity:
-
Damage the gut lining
-
Mimic hormones and disrupt thyroid or adrenal function
-
Create oxidative stress and chronic inflammation
-
Trigger immune attacks through mimicry
How to reduce your toxic load:
-
Choose organic when possible
-
Use glass or stainless steel instead of plastic
-
Avoid synthetic fragrances
-
Support detox with leafy greens, fiber, water, and herbs like milk thistle
-
Make sure you’re eliminating waste daily (yes, regular bowel movements matter)
Quick Recap: Toxins and Chemicals
-
Toxins add stress to your immune system and gut
-
Found in food, air, water, and everyday products
-
Gentle detox and cleaner choices go a long way
 7. Mental and Emotional Stress: The Autoimmune Accelerator
7. Mental and Emotional Stress: The Autoimmune Accelerator
Stress isn’t just mental. It has real, physical effects on the immune system, hormones, and gut. Chronic stress keeps the body in survival mode, which makes healing nearly impossible.
Stress affects autoimmunity by:
-
Increasing cortisol, which can suppress then dysregulate the immune system
-
Making the gut more permeable
-
Disrupting sleep and hormone cycles
-
Lowering your ability to repair and recover
Common signs of chronic stress:
-
Trouble sleeping
-
Mood swings or anxiety
-
Muscle tension or jaw clenching
-
GI issues during emotional times
-
Feeling wired but tired
Supportive tools:
-
Breathwork, meditation, and mindfulness
-
Therapy or coaching
-
Journaling or creative expression
-
Regular time in nature
-
More rest and joy in your schedule
Quick Recap: Mental and Emotional Stress
-
Chronic stress fuels inflammation and gut damage
-
Mind-body tools are key to healing
-
Emotional wellness supports physical recovery
 8. Adrenal Fatigue: Burnout at the Root of Immune Imbalance
8. Adrenal Fatigue: Burnout at the Root of Immune Imbalance
The adrenal glands help regulate energy, stress, and inflammation. When overworked, they can’t keep up, leading to fatigue, brain fog, and poor immune resilience.
How adrenal dysfunction affects autoimmunity:
-
Cortisol becomes imbalanced, leading to flares
-
Thyroid function may drop
-
You become more reactive to stress and illness
-
Recovery feels harder and slower
Signs of adrenal fatigue:
-
Exhaustion even with rest
-
Brain fog
-
Dizziness when standing
-
Cravings for salt or sugar
-
Afternoon energy crashes
-
Wired at night, tired in the morning
Supportive steps:
-
Prioritize deep rest and quality sleep
-
Eat protein and fat regularly
-
Cut back on caffeine
-
Use gentle adaptogens with guidance
-
Build recovery into your routine
Quick Recap: Adrenal Fatigue
-
Overworked adrenals can trigger autoimmune flares
-
Linked with fatigue, low resilience, and poor stress response
-
Nourishing and resting the body is key
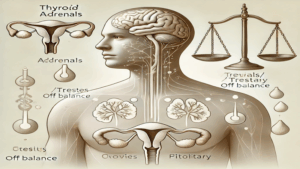 9. Hormone Imbalance: The Final Piece of the Puzzle
9. Hormone Imbalance: The Final Piece of the Puzzle
Hormones guide immune function, energy, and repair. Imbalances in estrogen, progesterone, thyroid, or cortisol can disrupt immune regulation and trigger autoimmunity—especially in women.
Common hormone-related factors in autoimmunity:
-
Thyroid issues (like Hashimoto’s or Graves’)
-
Estrogen dominance
-
Low progesterone
-
Perimenopause and menopause changes
-
Low testosterone
Signs of hormone imbalance:
-
Irregular or painful cycles
-
Low libido
-
Fatigue and weight gain
-
Mood swings
-
Sleep disturbances
Supportive strategies:
-
Balance blood sugar
-
Support the liver (hormones detox through the liver)
-
Eat healthy fats to build hormones
-
Avoid endocrine-disrupting chemicals
-
Consider testing and targeted support
Quick Recap: Hormone Imbalance
-
Hormones regulate immune balance
-
Imbalances can trigger or worsen autoimmunity
-
Healing starts with blood sugar, liver, and lifestyle support
Wrapping It All Together: Why This Holistic Framework Matters
Autoimmune disease doesn’t happen overnight, and healing isn’t about one magic fix. It’s about looking at the full picture. These nine root causes are often deeply connected, which is why addressing them together is so effective.
In my upcoming course, A Holistic Approach to Autoimmune Disorders, we’ll dive deeper into each of these areas with step-by-step strategies, healing protocols, mindset tools, and nutritional guidance to help you feel empowered and supported every step of the way.
You're not broken. Your body is trying to protect you. Let’s help it do that, the right way.